Contents
What are per and polyfluoroalkyl substances (PFAS)?
How could I be exposed to PFAS?
What are the health effects from exposure?
Can PFAS affect my pets and livestock?
Can I have my drinking water tested for PFAS?
Is it safe to eat produce grown in my home garden affected by PFAS?
Is it safe for my livestock to graze on land affected by PFAS?
What are regulatory agencies doing to address PFAS?
Introduction
Exposure to per- and polyfluoroalkyl substances (PFAS) is an emerging issue of concern for North Carolina and its residents. The occurrence of PFAS may have significant effects on our health and the environment.
This Extension publication is a guide to understanding and addressing PFAS in our households and communities. Information in this publication may be helpful for Extension agents, community members, and others who are interested in learning more about PFAS and their potential impact on our lives.
This publication addresses the following questions:
- What are per- and polyfluoroalkyl substances (PFAS)?
- How could I be exposed?
- What are the possible health effects from exposures?
- Can I have my water or soil tested for PFAS?
- Is it safe to eat from a home garden affected by PFAS?
- Is it safe for my livestock to graze on land affected by PFAS?
- How can we reduce our exposure?
- How are regulatory agencies addressing PFAS?
In addition, this publication concludes with a list of resources.
What are per- and polyfluoroalkyl substances (PFAS)?
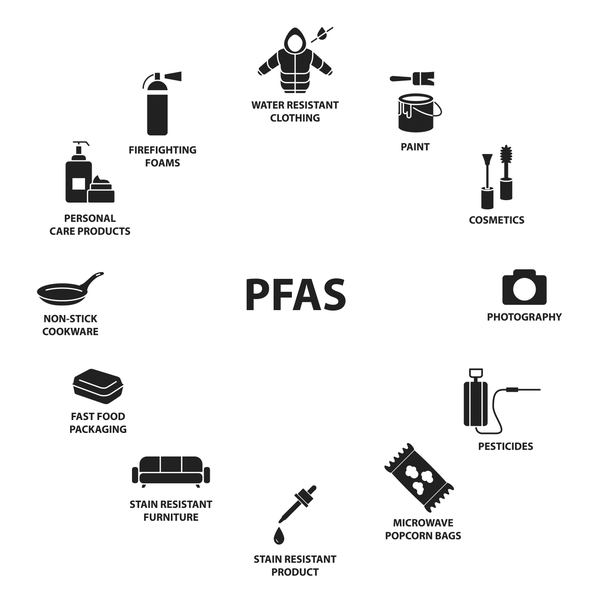
PFAS are a large group of chemicals that have been manufactured since the 1940s and continue to be widely used in household products today such as cosmetics, non-stick cookware, waterproof clothing, food packaging, and firefighting foams (Figure 1). Many PFAS have interesting, useful properties that include heat, water, or oil-resistance. These same properties make PFAS easy to transport in the environment and also difficult to degrade. In fact, PFAS have been called forever chemicals because they can build up and remain in the environment and our bodies for years (EPA 2023a, NC DEQ 2023b).
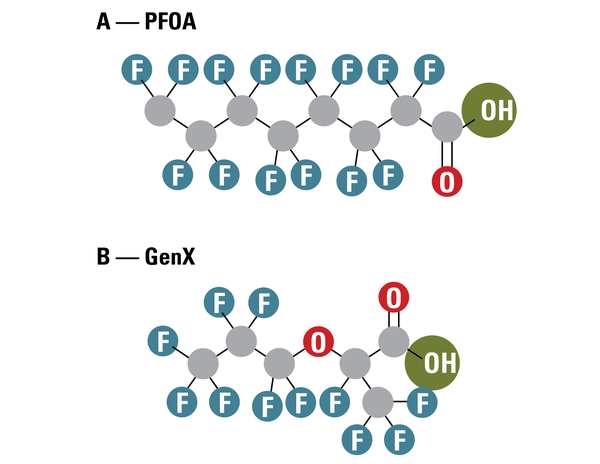
Today, there are more than 14,000 different PFAS in use, many of which behave uniquely in the environment and our bodies (EPA 2021, 2023d). Perfluorooctanoic acid (PFOA) and perfluorooctane sulfonate acid (PFOS) are two of the most widely used and investigated types of PFAS. These PFAS are called legacy PFAS because they are among some of the first PFAS in use. The legacy PFAS are also called long chain PFAS because of their molecular structure. Figure 2A shows the molecular structure of PFOA, which has eight carbon atoms attached to fluorine atoms and is commonly called C8. Both PFOA and PFOS have been phased out of production, and have been replaced gradually by thousands of other PFAS (EPA 2023a). Many replacement PFAS (such as GenX) are known as short chain PFAS because their molecular structure is different from PFOA and PFOS (Figure 2B).
Although we are in the early stages of understanding the extent of health effects from PFAS exposure, recent studies have warned that exposure to PFAS, even at low concentrations, may be linked to serious health effects.
How could I be exposed to PFAS?
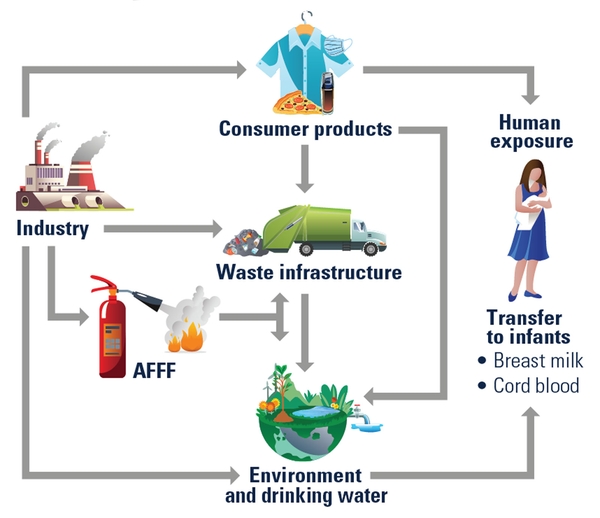
PFAS are so widely used that they are found in the environment around the world (Sunderland et al. 2019). Most individuals in the United States have been exposed to PFAS during their lifetimes, and the chemicals are detectable in the blood of most Americans (Lewis et al. 2015). Most individuals are exposed to PFAS through drinking water. Surface water and/or groundwater become contaminated with PFAS, and then enter the public water systems and private wells that residents rely on for drinking water (NC DHHS 2023). Residents who live near industries or sites contaminated with PFAS have a greater chance of having contaminated drinking water. According to the Environmental Protection Agency (EPA), most standard water treatment processes do not have the ability to remove PFAS (EPA 2021).
Although water is the predominant path through which most individuals are exposed to PFAS, there are other exposure routes, such as eating foods grown in contaminated soil or fish from contaminated water and by breathing or swallowing PFAS-contaminated soil or dust. In addition, individuals can be exposed by using consumer products with PFAS (ATSDR 2023a). Those who work in industries that produce or use PFAS, such as manufacturing facilities or the fire service, may be exposed at greater rates than others (EPA 2023a). Figure 3 shows the main exposure routes to PFAS.
What are the health effects from exposure?
Although research is still in its early stages, there are health effects that have been linked to PFAS exposure. These include:
- Increased cancer risk: Several studies have reported an association between PFAS exposure and increased risk of some cancers, such as kidney and testicular cancer.
- Effects on reproduction: PFAS exposure has associated effects on reproduction, including increased rates of infertility.
- Effects on liver and thyroid glands: Studies have also reported an association between PFAS exposure and liver damage, changes in liver function, and changes in the levels of thyroid hormone.
- Effects on childhood development and behavior: Exposure to PFAS has been linked to developmental issues in children that include reduced birth weight, delayed cognitive development, and changes in hormone levels.
- Weakened immune function: Some studies have suggested that exposure to PFAS may weaken the immune system and increase individual susceptibility to infections.
- Increased risk of obesity: Exposure to PFAS has been associated with increased body weight and body mass index in both adults and children. (ATSDR 2023b; EPA 2023a)
The effects of PFAS exposure may depend on how often, how long, and how high the levels are, in addition to personal factors as age, sex, and overall health (NC DHHS 2023). Children may be more vulnerable than adults, given their higher rates of consumption of food and water relative to their body weight. To fully understand the extent of health effects from exposure to the thousands of PFAS currently in use, much more research is needed.
It is important to note that information on the health effects of PFAS is still evolving. Studies that can definitively demonstrate the links between PFAS exposure and health effects require many years to complete. In the meantime, many health organizations recommend minimizing exposure to PFAS as a precautionary measure. The following sections describe the actions of regulatory agencies in addressing PFAS and steps you can take to reduce your exposure.
Can PFAS affect my pets and livestock?
Pets and livestock animals may be exposed to PFAS in similar ways as humans. For example, pets and livestock may drink contaminated water or consume contaminated food or feed. Recent studies that detected PFAS in pets (such as cats and dogs) and livestock (such as cattle, horses, and chickens) found that PFAS uptake was linked to the consumption of contaminated drinking water and/or feed (Brake et al. 2023; Guruge et al. 2008; Hill et al. 2022; Rock et al. 2023; Vestergren et al. 2013). Other studies found that PFAS can also transfer from exposed animals to their offspring as well as animal products, such as milk and eggs (Death et al. 2021). In addition, PFAS have been found to accumulate through the food chain in different animal species and are dependent on factors such as PFAS chemical properties, species, grazing behaviors, and habitat (Brake et al. 2023; Death et al. 2021; Mikkonen et al. 2023). Specific exposure routes and how they relate to the contamination of feed, drinking water, and environmental sources are not well understood and are an active area of current research (Mikkonen et al. 2023).
Most research on PFAS exposure and the health effects in pets and livestock has focused on PFOA and PFOS, the two legacy PFAS that are no longer in use. This means that we do not have a solid understanding of how the thousands of other, newer PFAS may affect pet and livestock health (Brake et al. 2023). Studies that have been conducted to date have shown that the main health effects on animals are related to effects on liver and thyroid function as well as other developmental and reproductive effects (Brake et al. 2023; Michigan PFAS Action Response Team 2023b). Organizations currently recommend limiting your pet’s and livestock’s exposure to PFAS until more information is available.
Can I have my drinking water tested for PFAS?
Drinking water is one of the primary ways in which humans and animals are exposed to PFAS. If you wish to have your drinking water tested for PFAS, the steps to take depend on the source of your water and your location.
Households in the Cape Fear River Basin of North Carolina may be eligible for free sampling and testing of their water if they meet the following criteria:
- If you are a resident of Bladen, Cumberland, Robeson, or Sampson counties, and you live near the Chemours Company facility (defined as 10 miles south and 25 miles north of the facility), you may be eligible to have your drinking water tested for PFAS at no cost. Contact Chemours at 910-678-1101 for further information on testing your drinking water for PFAS.
- If you are a resident of Brunswick, Columbus, New Hanover, or Pender counties, you may be eligible to have your drinking water well sampled for PFAS at no cost. Contact Chemours at 910-678-1101 or complete their online form (Private Drinking Water Well Information Request) for further information on testing your drinking water well for PFAS.
In both cases, the sampling and analyses are conducted by a certified, third-party environmental consultant, and not the chemical company.
If you live outside the Cape Fear River Basin, or do not meet these criteria, you may take the following steps:
- Households connected to a municipal water supply should first contact the local water utility to inquire if they have, or plan to, test for PFAS, and if they are taking steps to address PFAS in their drinking water supply.
- You can request that a certified lab test your drinking water for PFAS (NC State-Superfund 2022). The NC DHHS has compiled a list of certified labs that conduct tests for PFAS in drinking water (Table 1).
- The North Carolina Department of Environmental Quality (NC DEQ) has a list of certified labs for PFAS testing in surface and groundwaters for both in-state testing and out-of-state testing. See the Certified Laboratory listing. Costs range from $300 and $600 to test for PFAS in drinking water.
- If you rely on a private well, remember that there are many other routine tests that you should have done. Consider the well testing recommendations of the NC DHHS and your local health department as you seek PFAS testing. For example, Wake County provides information on PFAS and water quality testing for private well users on their Well Water Testing—PFAS Information page.
Agricultural producers can also request PFAS testing in water through a federal program associated with the US Department of Agriculture (USDA). The Conservation Evaluation and Monitoring Activity (CEMA) 209 offers testing to detect and measure PFAS in water and soil. This provides producers with a prescreening level of PFAS at their agricultural operation (USDA 2022). For more information on USDA’s programs to test PFAS in water and soil:
Is it safe to eat produce grown in my home garden affected by PFAS?
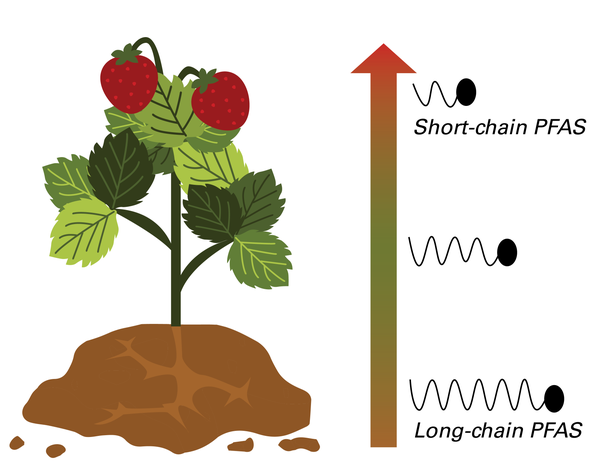
Studies have found that some plants can take up PFAS from contaminated water or soil. Plant uptake depends on the type and concentration of PFAS, type of plant, soil properties (such as organic carbon and soil amendments), frequency of precipitation or irrigation, and part of plant to be consumed (such as fruits or leaves) (Minnesota Department of Health 2022; Michigan PFAS Action Response Team 2023a).
There is insufficient information available to predict how much PFAS will be taken up by a specific plant or those grown in home gardens. However, some studies have suggested that longer-chain PFAS compounds may remain in plant roots, while shorter-chain PFAS may travel to other parts of the plant such as the leaves and fruit (Ghisi et al. 2019). (See Figure 5.) In addition, higher concentrations of PFAS in the soil and water used for growing the plants are related to higher concentrations of PFAS in the plants themselves (Wisconsin Department of Health Services 2023).
There are currently no safety threshold values for PFAS in edible plants, including both those commercially produced or those grown in home gardens. Potential health risks of consuming edible plants in home gardens that are contaminated with PFAS may depend on which PFAS is present, the quantity that is present, and the type and quantity of plant consumed. In addition, personal factors such as age, sex, and overall health can contribute to risk (NC DHHS 2023).
Is it safe for my livestock to graze on land affected by PFAS?
Currently, there are no safety standards for PFAS in soil used for agriculture, including soil for growing animal feed, grazing, or foraging for livestock. Several factors known to influence the risk to livestock from PFAS in agricultural settings include:
- The type of farm or operation
- Type of livestock
- Livestock grazing or feeding habits
- Source(s) of drinking water for livestock
- Current and historical land uses, including the use of biosolids
- PFAS concentration in soil or water sources (Mikkonen et al. 2023).
More research is needed to understand the risks of livestock grazing on or near land affected by PFAS. If your farm or operation is known or suspected to be affected by PFAS contamination by drinking water sources or soil amendments, you may wish to take precautionary measures to reduce your livestock’s exposure. These measures include using drinking water for livestock that follow the same safety standards as humans, modifying farming practices such as livestock rotation and timing to reduce exposures prior to finishing livestock, and using supplemental feed or water sources if rotation is limited (Mikkonen et al. 2023). In addition, you should contact a veterinarian if your livestock have been exposed to PFAS and are experiencing liver, kidney, immune, or reproductive issues (Michigan PFAS Action Response Team 2023a,b).
What are regulatory agencies doing to address PFAS?
After extensive research on PFAS, U.S. government agencies have begun to act. In 2023, the Environmental Protection Agency (EPA) proposed new regulations for six PFAS in public water systems (EPA 2023b), under the National Primary Drinking Water Regulation (NPDWR). The EPA proposed a maximum contaminant level (MCL) for PFOA and PFOS of four parts per trillion (ppt). The MCLs are the highest concentration of a contaminant that is allowed in drinking water at the water treatment plant. EPA’s NPDWR will also regulate four other PFAS chemicals, including GenX, PFNA, PFHxS, and PFBS. For these PFAS, a hazard index calculation is used to estimate if the combined concentrations pose a risk to human health.
If finalized, the proposed rule will go into effect in three years. In addition to regulation of these six PFAS in drinking water, the EPA also issued lifetime drinking water health advisory levels for GenX and PFBS at 10 ppt and 2,000 ppt, respectively. Health advisory levels are unenforceable guidelines that represent the concentration of a contaminant in drinking water from which no adverse health effects are expected to occur (EPA 2023b).
The EPA also published a strategic roadmap that outlines other federal activities that address PFAS (EPA 2023c). These activities include a proposal to designate PFOA and PFOS as hazardous substances under the Comprehensive Environmental Response, Compensation, and Liability Act (CERCLA or Superfund), which would provide funds for the cleanup of contaminated sites. Other federal activities in the roadmap include revising guidelines to reduce upstream PFAS discharges (such as industrial facilities involved in PFAS production and processing, metal finishing, airports, pulp and paper production, landfills, and textile and carpet manufacturing), completing a risk assessment of PFOA and PFOS in biosolids (projected for 2024), improving public access to PFAS chemical data and safety information, and providing public access to PFAS analytic tools for the reporting, testing, and occurrence of PFAS in communities (EPA 2023c).
Also at the federal level, the USDA is offering supplemental PFAS testing for water or soil to agricultural producers (including farmers) to help determine if PFAS are affecting their agricultural operations (White House 2023). In addition, USDA has created a dairy indemnity payment program that provides compensation for producers who have contaminated milk and milk products, and cows with negative effects from PFAS (USDA 2021). The USDA’s Food Safety and Inspection Service (FSIS) has also been working with the Food and Drug Administration (FDA) to conduct surveillance sampling of meat, poultry, and seafood products, while the FDA continues to monitor PFAS concentrations in different foods in the US food supply (White House 2023).
In North Carolina, the Department of Environmental Quality (NCDEQ) released an action strategy for PFAS in 2022 that included three key areas: 1) protecting communities from exposures to PFAS, 2) protecting drinking water sources through regulatory standards and pollution prevention, and 3) cleaning up contaminated sites that may affect human health and drinking water sources. Also in 2022 and over a three-month period, the NC DEQ tested 50 different municipal and county water systems that were associated with higher rates of PFOA and PFOS contamination over a three-month period. For details, see the DEQ Sampling of Public Water Systems.
In addition to sampling water systems, the NC DEQ is collecting discharge information to better understand exposures through emissions (such as air and water emissions from industrial sites) and health effects from PFAS exposures (NC DEQ 2022). The NC DEQ is developing emission permit conditions across the state and has begun requiring the disclosure of emission and discharge data (NC DEQ 2023b). For details on how DEQ is addressing these actions, see the DEQ Action Strategy for PFAS (PDF, 2.0 MB). In the coming months, the NC DEQ has also proposed to develop and introduce PFAS regulatory standards for ground and surface waters as well as drinking water standards (such as MCLs) (NC DEQ 2022). These standards are expected to be a combination of enforceable regulations and voluntary actions. Further, the NC DEQ is also developing remediation goals for PFAS contaminated sites. Finally, the NC DHHS recently introduced recommended limits on the consumption of certain freshwater fish found in the middle and lower Cape Fear River after detecting elevated levels of multiple PFAS, including PFOS, in fish collected from these areas. Similar to North Carolina, other states have begun setting regulatory limits for PFAS due to potential health and environmental concerns.
What can I do to reduce my exposure to PFAS?
One of the first steps to reducing your exposure to PFAS is reducing exposure through drinking water. (See previous sections for details on testing your water to determine PFAS concentrations.) For households in the Cape Fear River Basin, out of an abundance of caution, it should be assumed that PFAS are present in drinking water until testing confirms either the presence or absence of PFAS. As described in the sections above, there are free testing programs available for residents of the Cape Fear River Basin that are provided by third party, environmental consultants. In addition, agricultural producers may also be able to request PFAS testing in water and soil through a federal program associated with the USDA (CEMA 209).
If you have confirmed the presence of PFAS in your drinking water, you may wish to reduce your exposure by installing an in-home filtration system. In the NCDHHS publication on selecting a water treatment system (PDF, 1,390 KB), the agency describes technologies and commercial brands that may be effective in removing PFAS in drinking water by either reverse osmosis or activated carbon filters. Depending on where you live, if you receive your water from a municipal system or a well, and the types and concentrations of PFAS in your water, you may wish to consult with a professional about which filtration option best meets the needs of your household. Well users should also test their water for naturally occurring contaminants, such as uranium and radon in water, to determine the best treatment option.
PFAS exposure can also be reduced by avoiding foods that contain PFAS such as fish or other seafood caught in PFAS-contaminated water. In fact, the NC DHHS recently issued a fish advisory that provided safe consumption recommendations for fish species in the middle and lower Cape Fear River due to PFOS contamination (Table 2). A fish species that is not listed may not indicate the absence of PFAS. Instead, there may not be sufficient data to issue a recommendation for that species. Similarly, the Agency for Toxic Substances and Disease Registry (ATSDR) recommends avoiding food grown or raised near sites that have made or used PFAS (ATSDR 2023a).
You may also wish to reduce the amount of PFAS-containing products that you use at home. For example, it may be useful to be conscious of purchasing choices the next time you purchase items such as choosing stainless steel or cast iron cookware instead of nonstick cookware that may contain PFAS. You can also limit your exposure to PFAS by reducing or eliminating the use of food packaging that is likely to contain PFAS (such as grease-resistant paper found in fast food containers or wrappers, microwave popcorn bags, or pizza boxes) or water-resistant clothing (such as waterproof jackets and pants). Several companies have committed to not using PFAS in their products, which can help guide your purchasing choices: PFAS Central—PFAS-Free Products.
Finally, given how widespread PFAS use has been, it may be difficult to eliminate all exposure. In the long term, it is most important to support policies and decisions that will reduce or limit the use of PFAS to products in which they are essential or not easily replaceable.
How can I learn more?
If you are interested in learning more about PFAS and how to protect yourself or your community from potential exposures, the following resources may be helpful.
- Agency for Toxic Substances and Disease Registry (ATSDR) resources:
- Environmental Protection Agency (EPA) resources:
- North Carolina Department of Environmental Quality (NC DEQ) resources:
- North Carolina Department of Health and Human Services (NC DHHS) resources:
- NC State Center for Environmental Health Effects of PFAS:
- NC State Extension publications on understanding risk:
- Grieger, K., Horgan, M. Cummings, C. 2023. Let’s Talk About Risk: A Guide to Identifying, Assessing, Managing, and Communicating Risk. NC State Extension Publication AG-945.
- PFAS Central: PFAS-Free Products
- United States Department of Agriculture (USDA) resources:
- United States Food and Drug Administration (US FDA) resources:
- Wake County, North Carolina resources:
References
Agency for Toxic Substances and Disease Registry (ATSDR). 2023a. “PFAS and Your Health.” Washington: U.S. Department of Health and Human Services. ↲
Agency for Toxic Substances and Disease Registry (ATSDR). 2023b. “What are the Health Effects of PFAS?" Washington: U.S. Department of Health and Human Services. ↲
Brake, Heather D., Antonia Langfeldt, John B. Kaneene, and Melinda J. Wilkins. 2023. “Current Per- and Polyfluoroalkyl Substance (PFAS) Research Points to a Growing Threat in Animals.” Journal of American Veterinary Medical Association 261, no.7: 952-958. ↲
Death, Claire, Cameron Bell, David Champness, Charles Milne, Suzie Reichman, and Tarah Hagen. 2021. “Per- and Polyfluoroalkyl Substances (PFAS) in Livestock and Game Species: A Review.” Science of the Total Environment 774: 144795. ↲
Environmental Protection Agency (EPA). 2021. “National PFAS Testing Strategy: Identification of Candidate Per- and Poly-fluoroalkyl Substances (PFAS) for Testing.” Washington: EPA. ↲
EPA. 2023a. “Our Current Understanding of the Human Health and Environmental Risks of PFAS.” Washington: EPA. ↲
EPA. 2023b. “Proposed PFAS National Primary Drinking Water Regulation.” Washington: EPA. ↲
EPA. 2023c. “PFAS Strategic Roadmap: EPA’s Commitments to Action 2021 – 2024.” Washington: EPA. ↲
EPA. 2023d. “CompTox Chemicals Dashboard v2.2.1.” Washington: EPA. ↲
Ghisi, Rosselli, Telofilo Vamerali, and Sergio Manzetti. 2019. “Accumulation of Perfluorinated Alkyl Substances (PFAS) in Agricultural Plants: A Review.” Environmental Research 169: 326-341. ↲
Guruge, Keerthi S., Pathmalal M. Manage, Noriko Yamanaka, Shirgero Miyazaki, Sachi Taniyasu, and Nobuyoshi Yamashita. 2008. “Species-Specific Concentrations of Perfluoroalkyl Contaminants in Farm and Pet Animals in Japan.” Chemosphere 73, no.1(supplement): S210–S215. ↲
Hill, Nicholas, Jitka Becanova, and Rainier Lohmann. 2022. “A Sensitive Method for the Detection of Legacy and Emerging Per- And Polyfluorinated Alkyl Substances (PFAS) in Dairy Milk.” Analytical and Bioanalytical Chemistry 414, no. 3:1235-1243. ↲
Lewis, Ryan C., Lauren E. Johns, and John D. Meeker. 2015. “Serum Biomarkers of Exposure to Perfluoroalkyl Substances in Relation to Serum Testosterone and Measures of Thyroid Function among Adults and Adolescents from NHANES 2011–2012.” International Journal of Environmental Research and Public Health 12, no. 6: 6098–6114. ↲
Michigan PFAS Action Response Team. 2023a. “PFAS and Biosolids / Land Applications.” State of Michigan: Michigan.gov. ↲
Michigan PFAS Action Response Team. 2023b. “PFAS and Pets and Livestock Health.” State of Michigan: Michigan.gov. ↲
Minnesota Department of Health. 2022. “Per- and Polyfluoroalkyl Substances (PFAS).” St. Paul: MN Department of Health. ↲
National Institute of Environmental Health Sciences (NIEHS). 2019. “PFAS Fact Sheet.” Research Triangle Park: National Institutes of Health.
NC Department of Environmental Quality (NC DEQ). 2022. “Action Strategy for PFAS.” Raleigh: NCDEQ. ↲
NC DEQ. 2023a. “DEQ PFAS Sampling of Public Water Systems.”Raleigh: NCDEQ.
NC DEQ. 2023b. “Understanding PFAS.” Raleigh: NCDEQ. ↲
NC Department of Health and Human Services (NC DHHS). 2023. “Epidemiology: Occupational and Environmental - PFAS.” Raleigh: NC DHHS. ↲
NC DHHS. 2023. “NC DHHS Recommends Limiting Fish Consumption from the Middle and Lower Cape Fear River Due to Contamination with ‘Forever Chemicals.’” Raleigh: NC DHHS. ↲
NC State University. 2023. “Center for Environmental and Health Effects of PFAS.” Raleigh: NC State.
NC State University. 2022. “Superfund.” Raleigh: NC State. ↲
NC PFAS Testing Network. 2023. “NC PFAS Testing Network.” North Carolina: NC PFAS Testing Network.
National Institute of Environmental Science. 2019. “PFAS Fact Sheet.” Washington: NIES.
Vestergren, Robin, Francis Orata, Urs Berger, and Ian T. Cousins. 2013. “Bioaccumulation of Perfluoroalkyl Acids in Dairy Cows in a Naturally Contaminated Environment.” Environmental Science and Pollution Research 20, no. 11: 7959–7969. ↲
Rock, Kylie D., Madison E. Polera, Theresa C. Guillette, Hanna M. Starnes, Kentley Dean, Mike Watters, Debra Stevens-Stewart, and Scott M. Belcher. 2023. “Domestic Dogs and Horses as Sentinels of Per- and Polyfluoroalkyl Substance Exposure and Associated Health Biomarkers in Gray’s Creek North Carolina.” Environmental Science and Technology 57, no. 26: 9567-9579. ↲
Sunderland, Elsie M., Xindi C. Hu, Clifton Dassuncao, Andrea K. Tokranov, Charlotte C. Wagner, and Joseph G. Allen. 2019. “A Review of the Pathways of Human Exposure to Poly- and Perfluoroalkyl Substances (PFASs) and Present Understanding of Health Effects.” Journal of Exposure Science & Environmental Epidemiology 29, no.2:131-147. ↲
United States Department of Agriculture (USDA). 2021. “Supplemental Dairy Margin Coverage Payment; Conservation Reserve Program; Dairy Indemnity Payment Program; Marketing Assistance Loans, Loan Deficiency Payments, and Sugar Loans; and Oriental Fruit Fly Program.” Docket ID FSA-2021-0003. Washington: National Archives and Records Administration. ↲
USDA. 2022. Conservation Evaluation and Monitoring Activity (CEMA) 209. Washington: USDA. ↲
United States Geological Survey (USGS). 2022. “What are Per- and Polyfluoroalkyl Substances (PFAS)?” Washington: USDS. ↲
Wisconsin Department of Health Services. 2023. “PFAS and Backyard Gardening: Facts and Tips for Home Gardeners in Areas with Known or Suspected PFAS Contamination.” P-0311. Madison: Wisconsin Department of Health Services. ↲
White House Council on Environmental Quality. 2023. “Biden-Harris Administration Progress on Per- and Polyfluoroalkyl Substances: Steps Taken and Ongoing Actions, White House Council on Environmental Quality, March 2023.” Washington: Executive Office of the President. ↲
Xu, Benuto, Shuai Lium, John L. Zhou, Chunmiao Zheng, Jin Weifeng, Bei Chen, Ting Zhang, and Wenhui Qiu. 2021. “PFAS and Their Substitutes in Groundwater: Occurrence, Transformation and Remediation.” Journal of Hazardous Materials 412: 125159. ↲
Authors
Khara Grieger: Assistant Professor and Extension Specialist, Environmental Health and Risk Assessment, Department of Applied Ecology, NC State University
Katy May, Co-Director, Community Engagement Core for the Center for Human Health and the Environment, and Director, Community Engagement Core for the Center for Environmental and Health Effects of PFAS, NC State University
Publication date: Jan. 18, 2024
AG-955
N.C. Cooperative Extension prohibits discrimination and harassment regardless of age, color, disability, family and marital status, gender identity, national origin, political beliefs, race, religion, sex (including pregnancy), sexual orientation and veteran status.